
By Christine H. Monahan and Linda J. Blumberg
As hospitals increase in measurement and scope, together with taking up outpatient well being care settings, costs for routine medical providers are rising, typically dramatically. It is a downside in each Medicare and the business insurance coverage market as a result of hospitals typically invoice further facility charges on prime of the skilled fees from the physicians or different practitioners who present care. Within the business market, the results of facility payment billing are compounded by the shortage of worth regulation limiting how a lot market-dominant hospitals and well being programs can cost. The rising measurement of deductibles, in addition to extra, distinct cost-sharing obligations for hospital and doctor payments, imply that customers typically instantly bear the brunt of those fees.
Over the previous a number of years, Congress and the Facilities for Medicare and Medicaid Companies (CMS) have taken preliminary steps to rein in facility payment billing in Medicare, however a lot of the issue stays. At present, Congress is contemplating a number of proposals (exhibit 1), most of that are bipartisan, to maneuver the ball ahead one other step. On this article, we take a better take a look at the present slate of proposals to reform abusive billing practices within the business market.
Exhibit 1: Present congressional proposals to reform or enhance transparency on facility payment billing below business well being plans
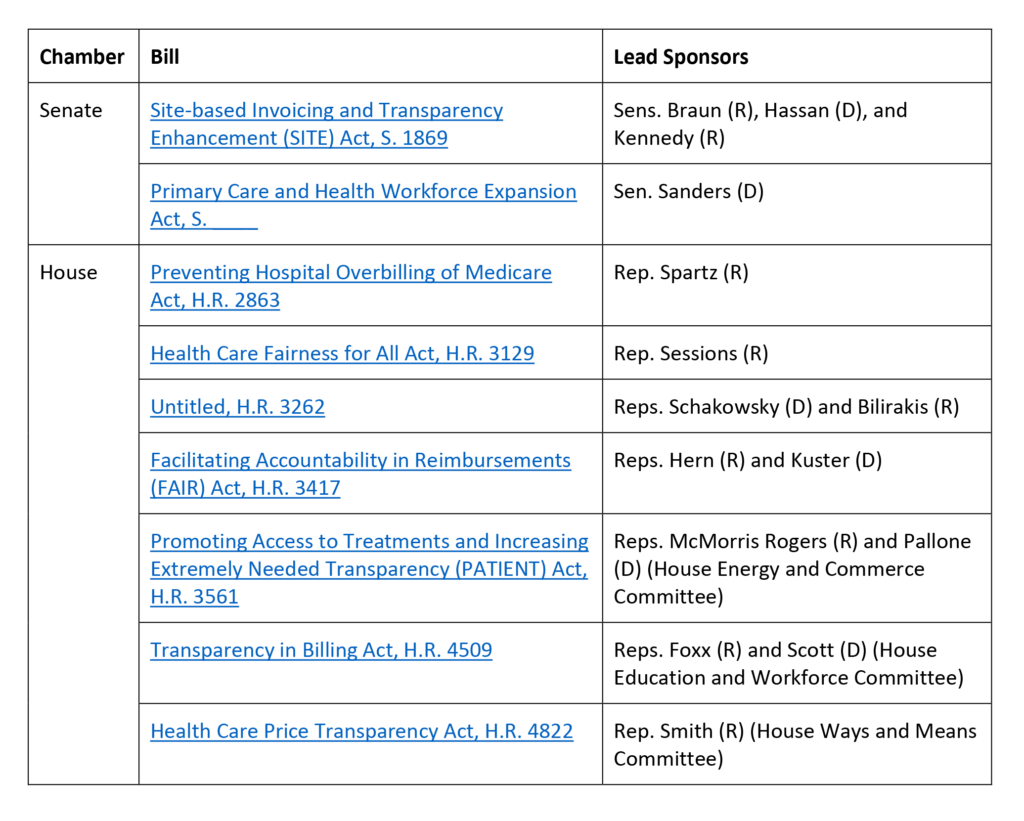
Supply: Authors’ evaluation.
Value Caps And Web site Neutrality In The Industrial Market
By far, probably the most complete invoice floated up to now is Senator Bernie Sanders’ (I-VT) Major Care and Well being Workforce Growth Act. What makes this invoice stand out is that it seeks to not solely curtail abusive outpatient facility payment billing within the business market, as some states have begun to do, but in addition would impose worth caps as a mechanism to attain site-neutral funds for a significant swathe of providers.
We’ve beforehand mentioned the restrictions of prohibiting outpatient facility payment fees with out together with extra pricing constraints. In brief, prohibiting hospitals from billing outpatient facility charges with none regulation of the whole costs charged permits hospitals with market energy to extend the charges their affiliated physicians and different well being care professionals cost for these providers and in any other case enhance costs for different providers to make up for the misplaced income. Though such reforms could generate short-term financial savings, they’re unlikely to meaningfully include prices within the longer run. Including worth caps, at the least for a specified set of low-complexity outpatient providers generally offered in doctor workplaces, would restrict hospitals’ means to extend skilled charges for outpatient providers past a specified stage. How excessive or low that cost is relative to present reimbursement ranges, in addition to how broadly it applies, will largely decide the potential value financial savings. These worth caps in the end could lead insurers to attain “web site neutrality,” paying the identical quantity for providers whether or not in a hospital or unbiased setting.
Sen. Sanders’ proposed worth caps would attain a comparatively broad set of providers: all care offered in off-campus outpatient settings in addition to low-complexity providers offered in on-campus settings, as long as they are often safely and appropriately furnished in off-campus settings as properly. This explicitly consists of analysis and administration providers and telehealth providers, in addition to different gadgets and providers to be decided by the secretary of Well being and Human Companies. This focus is just like proposals for site-neutral funds in Medicare from the Medicare Fee Advisory Fee and for limiting facility charges from the Nationwide Academy for State Well being Coverage.
In proposing a cost stage for these providers within the business market, Sen. Sanders is breaking new floor whereas drawing on an present idea: the No Surprises Act’s (NSA’s) qualifying cost quantity (QPA). Particularly, Sen. Sanders’ proposal would restrict suppliers and services to charging one payment that’s no better than the QPA for a lined merchandise or service. This side of the invoice is bound to ask debate; the calculation of the QPA below the NSA has confronted ongoing lawsuits by well being care suppliers and their supporters. It stays to be seen whether or not reliance on the QPA—and even the business worth ceiling proposal extra broadly—survives past this primary draft of Sen. Sanders’ invoice (which has but to be formally launched), however, even when not, Sen. Sanders has opened the door to dialogue and debate of a coverage strategy that warrants consideration.
Transparency In Billing
The remaining business market billing reforms in Congress deal with bettering transparency round outpatient facility payment billing. These proposals are pushed by a rising recognition that well being care payers, and the researchers, regulators, and coverage makers who depend on claims information, have a surprisingly poor understanding of the place care is offered, by whom, and at what whole value. For instance, claims types typically solely embody the tackle and nationwide supplier identifier (NPI) for hospital’s fundamental campus or billing workplace fairly than the off-campus web site of care. Discrepancies between the data on hospital claims (historically the UB-04 type, or the digital equal thereof) {and professional} claims (historically the CMS-1500 type, or the digital equal thereof) additionally make it tough to reliably affiliate hospital {and professional} payments for the service to determine the whole worth of care. Moreover, exterior of registries in particular person states reminiscent of Massachusetts, there’s a lack of publicly out there information monitoring hospital possession and management over outpatient suppliers and settings.
On account of these data gaps, even insurers with some market leverage could also be unable to successfully negotiate with suppliers on the whole worth paid for providers and can’t assess how a lot care is being offered in numerous settings and the way the prices evaluate throughout these settings. Insurers additionally could have extra problem capitalizing on new legal guidelines, reminiscent of in Texas, that prohibit anti-steering or anti-tiering clauses if they can’t reliably distinguish when care is being offered at completely different outpatient places owned by the identical well being system. Moreover, absent higher data, coverage makers face challenges evaluating the potential results of various reforms, and regulators could have problem imposing new legal guidelines in search of to rein in abusive outpatient billing practices.
Nearly all of the at the moment pending payments largely search to deal with the shortage of location-specific data for the location of care on claims types. All of them would require that hospital outpatient departments, as outlined by CMS below the Medicare program, receive a singular NPI and use this identifier for billing. This 10-digit code would allow payers and different analysts reviewing claims information to know the precise location the place care was offered, with out the identical threat of errors that counting on an tackle alone would introduce. (Moreover, merely requiring the situation’s tackle with out updating the NPI could lead to insurer programs rejecting the claims as a result of the tackle on the declare doesn’t match the tackle related to the listed NPI.)
To the extent billing transparency laws strikes ahead, Congress might want to iron out technical variations among the many present proposals. One concern is whether or not simply hospitals and services want to incorporate the location of care’s distinctive NPI on claims or if well being care professionals should embody this data as properly. Many of the laws focuses on hospital payments, however this misses out on an essential alternative. If the location of care’s distinctive NPI is constantly included on each hospital payments {and professional} payments, insurers and different analysts will likely be higher in a position to affiliate claims for a similar service and calculate the whole value of look after every.
Each the Home Power and Commerce Committee proposal from Representatives Cathy McMorris Rodgers (R-WA) and Frank Pallone (D-NJ) and the Home Methods and Means Committee proposal from Consultant Jason Smith (R-MO) require the distinctive NPI on Medicare billing types solely. Consultant Pete Periods’ (R-TX) Well being Care Equity for All Act requires solely that off-campus hospital outpatient departments purchase a singular NPI however doesn’t explicitly require that it’s used when claims are submitted. In distinction, different proposals explicitly prolong the requirement to be used of a singular NPI such that business claims can’t be paid with out it. Some, such because the Training and Workforce Committee’s invoice, even impose parallel necessities that insurers can not pay and customers should not accountable for claims that don’t embody the situation of care’s distinctive NPI.
Arguably, even a proposal that’s centered on Medicare may benefit the business market as a result of rules below the Well being Insurance coverage Portability and Accountability Act (HIPAA) require well being care suppliers to make use of their NPI on all customary transactions. Nonetheless, there’s cause to imagine payments explicitly extending this requirement to business claims and offering extra enforcement mechanisms may have higher compliance, and thus an even bigger impression. First, suppliers probably may argue that their unique, systemwide NPI continues to be legitimate and proceed to make use of that on business claims. Second, business insurers would wish to replace their claims processing programs to simply accept claims with the brand new distinctive NPIs, and so they could not discover the motivation to be sufficiently robust to take this step if the laws applies solely to Medicare billing. If Congress in the end pursues a Medicare-only reform, it might behoove CMS to amend the HIPAA rules or concern steering to make sure the brand new, distinctive NPI is required on all business claims as properly and push insurers to accommodate these modifications.
Whereas switching to distinctive NPIs is a important step to raised understanding location information, it might grow to be more durable for payers and researchers to see the system affiliation of the completely different places that at the moment are submitting claims. Payers and the broader public would considerably profit from a complete federal system for monitoring hospital possession and acquisitions, reminiscent of that proposed by Representatives Janice Schakowsky (D-IL) and Gus Bilirakis (R-FL). Ideally this method can be designed to enhance the distinctive NPI requirement, in order that hospitals and well being programs should report all of their affiliated distinctive NPIs and replace this data on a well timed foundation, on prime of different information necessities at the moment included within the invoice. To the extent such a proposal will not be adopted, CMS ought to think about how else it could possibly higher accumulate this data below present authorities—both leveraging information collected as a part of the NPI software or maybe newly gathering such data by means of hospitals’ Medicare value stories.
Wanting Ahead
The price penalties of present billing practices are substantial. Shoppers want lawmakers to start curbing this abusive habits that places them liable to greater value sharing and medical debt and will increase their premiums. The proposals pending earlier than Congress are a important first step, though exterior of Sen. Sanders’ invoice, they’re additionally solely that—extra centered on transparency of data on pricing than on lowering whole costs of low complexity providers.
Assuming we don’t see important expansions within the scope of those proposals in no matter package deal, if any, strikes ahead, it would fall on CMS, the states, and personal payers to maintain shifting the system ahead within the brief time period. However we must always not overstate the impression most of those proposals are more likely to have: Insurers in noncompetitive supplier markets have little to no leverage in negotiating decrease costs for providers, even when they can receive higher data on pricing. States are beginning to deal with this concern however face important opposition from the hospital trade. What’s extra, the first tactic states have pursued up to now—prohibiting facility payment fees for sure outpatient providers/settings—can lower shopper out-of-pocket prices however is not going to scale back whole prices as market-powerful hospitals make up their fees elsewhere, and premiums rise accordingly.
In the end, limits on whole costs for outpatient care, together with facility {and professional} fees, are essential to eradicate the expansion in these ballooning billing practices which have unfold broadly as a consequence of vertical integration in well being care.
Authors’ Be aware
On Wednesday, September 6, 2023, as this text went to manufacturing, Axios printed a dialogue draft floated by Republicans from the Home Methods and Means, Power and Commerce, and Training and Workforce Committees that may require Medicare hospital outpatient departments to acquire a singular NPI and use this for Medicare billing functions. The invoice is predicted to be launched imminently.
This submit is a part of the ongoing Well being Affairs Forefront sequence, Supplier Costs within the Industrial Sector, supported by Arnold Ventures.
Christine H. Monahan and Linda J. Blumberg, “Reforming Abusive Billing Practices, One Step At A Time,” Well being Affairs Forefront, September 8, 2023, https://www.healthaffairs.org/content material/forefront/reforming-abusive-billing-practices-one-step-time. Copyright © 2023 Well being Affairs by Undertaking HOPE – The Folks-to-Folks Well being Basis, Inc.