
By Sabrina Corlette and Karen Davenport
After a number of years of below-average will increase, premiums in employer-sponsored medical insurance are poised for charge hikes this 12 months. With this open enrollment season, staff will quickly know what premium will increase imply for his or her take-home pay and out-of-pocket prices, as at the very least some employers move elevated prices on to their staff.
There are greater than 15 million state and native authorities staff—those that work for state govt, judicial, or legislative department businesses, college districts, public universities and hospitals, or native municipalities—and so they too will really feel the pinch of elevated well being care prices. But, in some ways, the businesses that buy medical insurance for these public staff are uniquely located to sort out rising well being care prices. They’re usually the biggest industrial purchaser of well being care companies of their state and due to this fact have market energy to exert strain on insurance coverage corporations and suppliers. Moreover, given their dimension, their efforts to shift well being plan and supplier behaviors and encourage better efficiencies can have ripple results for different industrial purchasers. For these causes, many state lawmakers have seen these well being plans as a testing floor for well being coverage improvements. The Middle on Well being Insurance coverage Reforms’ (CHIR’s) latest survey of state worker well being plans (SEHPs) probed the important thing challenges dealing with these main well being care purchasers and recognized promising cost-control methods.
Costs Characterize Major SEHP Price Drivers
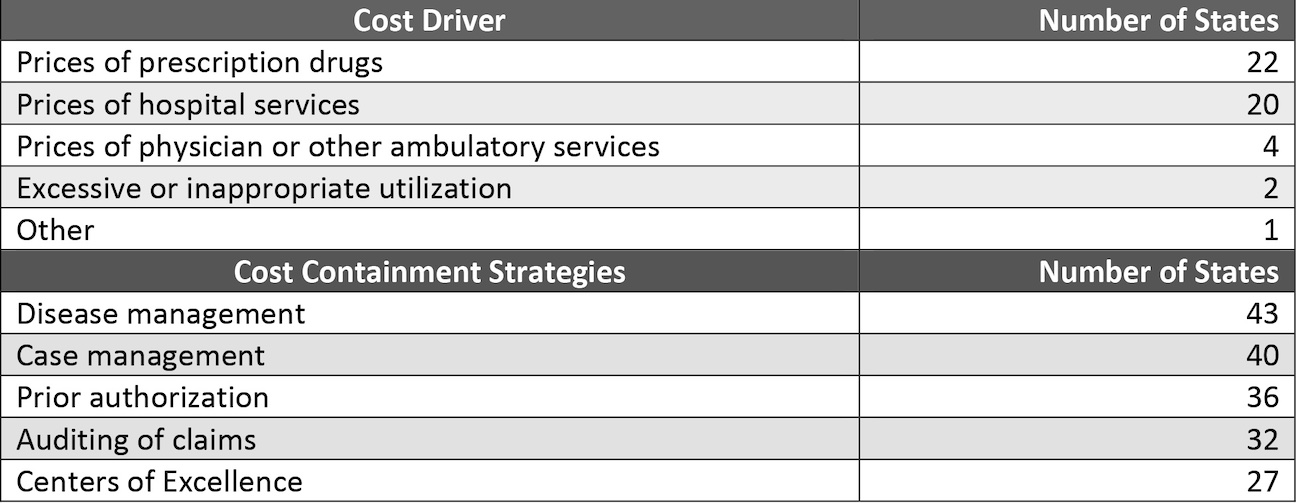
Within the CHIR’s 2023 survey, SEHP directors recognized prescription drug costs and costs for hospital companies as the first drivers of value progress. This discovering is in line with different surveys of private-sector employers. Only some SEHP directors cited different elements, resembling extreme or inappropriate use of well being care companies (exhibit 1). But, in the case of their cost-containment methods, most SEHPs prioritize curbs on enrollee use over controls on value progress. That is doubtless as a result of methods that focus on supplier costs can elicit resistance from each suppliers and plan enrollees and could be administratively difficult to implement—each sources of “friction” that plan directors search to reduce. This friction could assist clarify why, when requested to establish cost-control initiatives they’ve carried out over the previous 5 years, SEHPs generally reported new illness administration and case administration packages and prior authorization necessities. These approaches can imply staff with continual circumstances or acute well being care wants pay extra out of pocket or are denied protection for acceptable care.
Exhibit 1: Single highest value driver recognized in 2022 and high 5 cost-containment methods carried out over the previous 5 years
Promising Methods: Reference Pricing, Tiered Community Plans, And Multipayer Buying Initiatives
Whereas the vast majority of particular SEHP cost-control methods in our survey centered on decreasing use of well being care companies, roughly half the states additionally indicated that they’ve taken some steps to cut back hospital and ambulatory companies costs. And though no single technique concentrating on these value drivers emerged as a transparent favourite in our survey, follow-up interviews with SEHP directors surfaced promising outcomes for reference pricing, tiered community plans, and multipayer buying initiatives.
Reference Pricing
9 states in our survey reported pegging supplier funds to a reference value, resembling a share of Medicare’s fee for a particular service. Such packages have garnered consideration from coverage makers for the reason that Montana SEHP’s reference pricing initiative saved the state $47.8 million in hospital prices between state fiscal years 2017 and 2019. Extra just lately, an audit of 2021 claims knowledge for the Oregon state well being plan’s program revealed that the state had saved greater than $112.7 million, greater than initially projected.
In interviews, two SEHP directors with comparable reference pricing packages reported realizing vital financial savings with this easy-to-implement strategy. “We handle to save lots of about $40 million per 12 months,” famous an administrator in a state that units its costs primarily based on Medicare charges. The administrator additionally mirrored that though their reimbursement ranges should not as excessive as different industrial payers, they take pleasure in excessive supplier participation—99.3 % of hospitals and 80.0 % of physicians within the state take part of their community—which they attribute to the plan’s vital dimension and market presence.
Tiered Community Plans
Tiered community plans signify one other well-liked cost-control technique, with 14 SEHPs within the survey reporting that they provide a tiered community choice to their staff. Analysis on the price affect of tiered networks in personal medical insurance plans means that the usage of such networks can lead to modest however significant reductions in spending. For instance, one evaluation discovered that complete spending per member per quarter for enrollees in a tiered community plan fell by 5 %.
In these preparations, the well being plan divides suppliers into tiers primarily based on their efficiency towards high quality measures and spending targets; staff pay decrease value sharing to see suppliers within the high efficiency tier. SEHP directors respect the decrease prices—about 8 %, based on one state—that tiered community plans provide in comparison with a conventional broad and undifferentiated supplier community. In interviews, directors additionally famous that plan enrollees settle for tiered value sharing extra readily than a slim community that excludes high-price, however well-liked, well being methods.
Multipayer Initiatives
When well being care purchasers and payers collaborate and align their buying methods, it could possibly assist overcome a market dynamic during which consolidated, “must-have” supplier methods demand ever-higher costs for his or her companies. In our survey, solely 5 states reported that they’re collaborating with one other purchaser on cost-containment initiatives. California, New Mexico, and Washington State have coordinated with one other public purchaser, resembling Medicaid or the state-based Market, whereas Colorado and Maine have labored with private-sector purchasers. Particular examples embody a SEHP engaged on widespread requirements for well being plan efficiency with the Market and Medicaid businesses, one other SEHP working throughout payers to develop a brand new supply mannequin for rural hospitals within the state, and a 3rd SEHP that hopes to leverage multipurchaser alignment in value negotiations with massive hospital methods. “If all three businesses are working collectively on the identical issues, we’re going to have an unlimited affect,” predicted the SEHP administrator engaged on widespread plan efficiency requirements. This administrator additional noticed that their efforts to align throughout packages ease suppliers’ administrative and reporting burdens.
Takeaway
The expansion in common household premiums in employer-sponsored insurance coverage has steadily outpaced inflation and staff’ earnings. Household premiums are actually virtually $24,000 per 12 months. Many employers have tried to shift extra of those prices onto staff and their households via larger deductibles, with the end result that 43 % of individuals with employer-sponsored protection say it is vitally or considerably tough to afford their well being care, and greater than one-third of them battle with medical debt. On the identical time, many US employers acknowledge that well being care is an worker profit essential to recruiting and retaining a talented and productive workforce. Standing alone, nevertheless, most lack the capability and dimension to demand the fee and system adjustments essential to examine the expansion in well being care prices. State worker well being plans, nevertheless, usually have vital market energy, in the event that they select to make use of it.
Our survey finds that, whereas many SEHPs proceed to give attention to decreasing well being care use, quite a lot of SEHP directors are demonstrating that it’s doable to design and implement methods that cut back supplier value inflation whereas additionally minimizing pushback from necessary inner and exterior stakeholders. To the extent that a few of these methods change supplier habits or interact different well being care purchasers, enhancements in high quality or value financial savings can have ripple results throughout the marketplace for industrial insurance coverage. As these efforts garner extra expertise and knowledge, different SEHPs, in addition to private-sector purchasers and coverage makers, can be taught, and probably profit from, these initiatives.
This publish is a part of the ongoing Well being Affairs Forefront sequence, Supplier Costs within the Business Sector, supported by Arnold Ventures.
Sabrina Corlette and Karen Davenport, “In An Period Of Premium And Supplier Worth Will increase, State Worker Well being Plans Goal Key Price Drivers,” Well being Affairs Forefront, November 16, 2023, https://www.healthaffairs.org/content material/forefront/era-premium-and-provider-price-increases-state-employee-health-plans-target-key-cost. Copyright © 2023 Well being Affairs by Venture HOPE – The Individuals-to-Individuals Well being Basis, Inc.